Definition
“Palpitations are defined as an unpleasant perception of the heartbeat and are described by patients as a disagreeable sensation of throbbing or movement in the chest and/or adjacent areas.
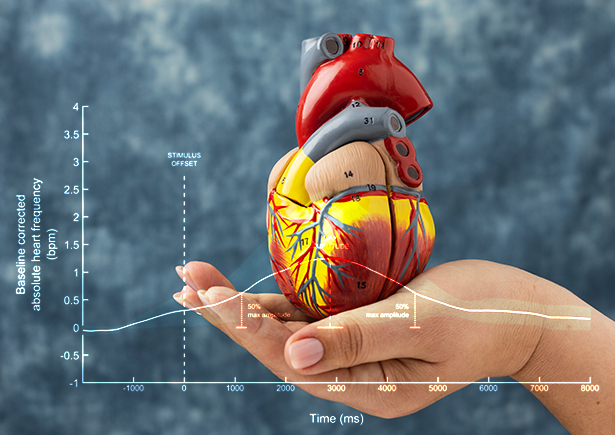
Mechanism
Alteration in heart rate |
Alteration in heart rhythm |
Augmentation of myocardial contraction |
Causes
Cardiac – 43 %, Psychiatric – 31 %, Miscellaneous – 10 %, Unknown – 16 %
The following are the causes of palpitations, based on causes described:
1. Palpitations due to arrhythmic causes
|
2. Palpitations due to structural heart disease
|
3. Palpitations due to systemic causes
|
4. Palpitations induced by drugs/illicit substances
|
5. Palpitations of psychiatric origin
|
Diagnostic Evaluation
- Age of onset
Inappropriate sinus tachycardia can occur at any age though more prevalent in young adults. Palpitations due to psychiatric causes are usually encountered in young adults. Palpitations due to accessory pathways (AVRT) predominate in childhood and adolescence and have a structurally normal heart.
AVNRT increases with age. Patients with palpitations due to VT tend to be older and usually with structural heart disease. - Description
The description of palpitations can give a clue to their origin as shown in this table:
Rapid and regular
Sinus tachycardia, SVT and VT
Rapid and irregular
Atrial fibrillation(AF), Multifocal Atrial Tachycardia(MAT), Atrial Flutter with varying block
Flip-flopping
Atrial/ventricular premature ventricular complexes(PVCs)
Rapid fluttering
SVT/VT
Rapid and Regular neck pulsations – Frog sign
AVNRT (systolic cannon waves which occur with AV dissociation result from simultaneous contractions of atria and ventricle against closed mitral and tricuspid valves causing reflux of blood into neck veins)
Irregular neck pulsations
AV dissociation in PVCs, complete heart block and VT(causes irregular systolic cannon waves due to varying relation between P and QRS due to atrioventricular dissociation)
- Onset and offset
This too helps to analyse the type of arrhythmia causing palpitations- Randomly and episodically and last for an instant – mostly premature beats
- Abrupt onset and offset – SVT or VT
- Gradual onset and offset – Sinus tachycardia
- Mode of termination : vagal stimulation – SVT
- Positional palpitations
- Palpitations upon standing up straight after bending over and ends by lying down – mostly AVNRT
- Intermittent pounding sensations on lying in bed – atrial or ventricular PVCs
- Palpitations associated with other symptoms
The accompanying symptoms of palpitations depend upon the underlying cause and the effect of palpitations on the coronary and cerebral blood flow.- Chest pain – Arrhythmogenic myocardial infarction
- Dyspnoea – Heart failure due to arrhythmias
- Syncope – low cardiac output during arrhythmias, hypoglycaemia, and pheochromocytoma
- Polyuria- SVT (due to release of atrial natriuretic peptide)
- Sweating – Anxiety, hypoglycaemia
- Diarrhoea, weight loss, increased appetite – Thyrotoxicosis
- Palpitations at rest or exertional
- Arrhythmic palpitations usually are gradual or sudden in onset and offset and usually occur at rest and rarely during exercise.
- Palpitations due to volume overload are related to exertion and disappear at rest.
- Any history of psychiatric diseases
- Anxiety
- Panic attacks
- Depression
- Somatization disorders
- Is there any history of underlying disease?
The main cause of palpitations is cardiac, and hence history pertaining to presence of underlying ischemic heart disease, rheumatic heart diseases, congenital heart diseases or cardiomyopathies must be elicited. A history of stressors or anxiety will help to diagnose psychiatric causes. Hypoglycaemia must be ruled out by context and thyrotoxicosis and pheochromocytoma can be diagnosed by typical clinical features. A drug history of intake of beta agonists, amphetamines, theophylline, may sometimes avoid unnecessary investigation. A history of alcohol intake must be recorded to rule out alcoholic cardiomyopathy or withdrawal from alcohol.
Clinical examination
The aim of clinical examination is to find out if the arrhythmia is life-threatening, causing hemodynamic compromise, or due to serious underlying heart disease.
The examination should begin with a recording of pulse rate and its regularity
Arrhythmia | Rate/regularity | JVP | BP | Other clinical features |
Atrial Fibrillation | 150-200/min Irregular | Absent “a” waves Absent ”x” descent | Hypotension in extreme rates | Varying volume of pulse Varying intensity of first heart sound Apex pulse deficit > 10 |
Atrial flutter | 200-250/min Regular Irregular if variable conduction
| Normal most of times as regular | Hypotension in extreme rates | May resemble atrial fibrillation if variable conduction occurs |
Atrioventricular block(CHB) | Significant bradycardia Regular | Irregular slow systolic cannon a waves | Patients may present with high blood pressure due to AV dissociation | Variable intensity of first heart sound |
AVNRT | 250-300/min Regular | Frog sign with rapid regular systolic cannon a waves(1:1 VA conduction) | Mostly normal | – |
VT | 250-300/min Regular | Irregular rapid systolic cannon a waves | With structural heart disease may present with hypotension
In structurally normal hearts , no hemodynamic compromise | Varying intensity of first heart sound
Systolic blood pressure unrelated to respiration |
Ventricular premature complexes | Variable Irregular | normal | normal | Apex pulse deficit < 10
Usually disappears with exercise
Premature beat followed by a compensatory pause |
The blood pressure is crucial in deciding the seriousness of any arrhythmia, as hypotension signifies reduced cerebral blood flow, due to compromise of cardiac output. In conditions with irregular heartbeat, BP may have to be recorded multiple times, and averaged, as in AF.
Patients with heart disease can be diagnosed by abnormal cardiac findings like cardiomegaly, murmurs, left and right heart failure must be documented, as this will help us decide further management.
Clinical features of thyrotoxicosis and pheochromocytoma, must be looked for in patients with normal hearts. Presence of cold extremities, and tremors, with anxious affect, may suggest a psychiatric basis for palpitation.
Evaluation in patient with Palpitations
- Standard 12 lead electrocardiography
Standard 12 lead ECG is an essential part of evaluation in all patients with palpitations. The suggestion of previous myocardial infarction may be a clue for significant arrhythmias, particularly ventricular tachycardia. Presence of left or right ventricular hypertrophy with atrial enlargement may point towards underlying chamber enlargement leading to volume overload. Nonspecific ST changes and T wave abnormalities are important clues to presence of myocardial diseases. A prolonged QT may suggest polymorphic VT whereas a short PR with delta waves may suggest underlying accessory pathway. Frequent premature ventricular complexes in a patient presenting with palpitations should always be localised and evaluated properly. - Routine blood Investigations
Baseline laboratory testing should include a complete blood count, blood sugar, blood urea nitrogen, serum creatinine, electrolyte levels and thyroid profile to exclude anaemia, renal disease, electrolyte and thyroid disorders, particularly thyrotoxicosis. Drug screening should be ordered in suspected cases presenting with palpitations. - Stress exercise testing
Patients with exertional symptoms should be evaluated with exercise testing because they are at higher risk of morbidity and mortality. Stress testing also provide prognostic value in some cases with palpitations. Patients with benign ventricular premature complexes can have disappearance of PVCs with exercise. Disappearance of pre-excitation on exercise testing (present on baseline ECG) may suggest a good prognosis in patients with WPW syndrome - Two Dimensional Echocardiography
Echocardiography should be considered a routine investigation in all patients with palpitations particularly when they are exertional. A high suspicion of abnormal test should be considered when patient has abnormal signs like elevated JVP and pedal edema. One should look for evidence of structural heart disease particularly regurgitant valvular lesions, underlying wall motion abnormalities, ventricular dysfunction and congenital heart diseases. - Ambulatory Holter monitoring
24-hour Holter monitoring should be considered when the patient experiences specific triggers or if symptoms tend to occur daily. If symptoms are less frequent, event loop recorders can be worn for longer period upto 30 days. Implantable loop recorders are subcutaneous devices in patients with infrequent palpitations accompanied by syncope concerning arrhythmic etiology. - Cardiac Imaging
Though not a frequently used modality, cardiac MRI may be a useful modality to know the underlying etiology in patients presenting with palpiations/syncope and PVCs on baseline ECG. Diseases like arrhythmogenic right ventricular dysplasia should be considered in patients with RVOT type of PVCs (LBBB morphology and positive VPC morphology in inferior leads) on baseline ECG. Other diseases like sarcoidosis, myocarditis and infiltrative diseases can also be diagnosed by cardiac MRI.
1.Electrocardiogram | Previous myocardial infarction Left or right ventricular hypertrophy Atrial enlargement Atrio-ventricular blocks Short PR and delta waves(WPW syndrome) Prolonged QT interval Isolated premature atrial/ventricular complexes |
2.Routine Investigations | Complete blood count BUN, Creatinine Blood sugar Thyroid profile Serum electrolytes Drug screen |
3.Exercise stress testing | Patients with palpitations on physical exertion or suspected coronary artery disease or myocardial ischemia |
4.Two dimensional Echocardiography | Rule out structural abnormalities/look for ventricular function |
5.Ambulatory 24 hour holter monitoring/Event loop recorders(maximum upto 30 days) | For patients with palpitations and structural heart disease.
In patients with family history of syncope, arrhythmia or sudden cardiac death |








