Best of ACC Updates
- 1.Empagliflozin After Acute Myocardial Infarction: EMPACT-MI
EMPACT-MI is double-blind, randomized, placebo-controlled trial, patients hospitalized for acute myocardial infarction and at risk for heart failure were assigned either empagliflozin (10 mg daily) or placebo within 14 days post- admission, alongside standard care.
Results from 3260 patients receiving empagliflozin and 3262 receiving placebo over a median follow-up of 17.9 months showed no significant difference in the primary endpoint, a composite of hospitalization for heart failure or death from any cause (8.2% in empagliflozin group vs. 9.1% in placebo group).
Analysis of individual components indicated a lower incidence of hospitalization for heart failure in the empagliflozin group but no significant difference in overall mortality compared to placebo.
Adverse events were consistent with the known safety profile of empagliflozin and comparable between groups - CSL112 (Apolipoprotein A-I) Infusions And Cardiovascular Outcomes In Patients With Acute Myocardial Infarction (ApoA-I Event Reducing In Ischemic Syndromes II (AEGIS-II) Trial)
The goal of the trial was to evaluate CSL112 apolipoprotein A-1 (apoA-1) infusion compared with placebo among patients with recent acute myocardial infarction (AMI). ApoA-1 increases cholesterol efflux capacity.
Results from 18,219 patients showed no significant difference between CSL112 and placebo groups in the risk of primary composite endpoint events at 90, 180, or 365 days of follow-up.
Adverse events were comparable between groups, although a higher incidence of hypersensitivity events was observed in the CSL112 group.
The suggestion of benefit among those with elevated baseline LDL-C is hypothesis generating. - A Double-blind, Randomized Placebo Procedure-controlled Trial Of An Interatrial Shunt In Patients With HfrEF And HfpEF: Principal Results From The RELIEVE-HF Trial
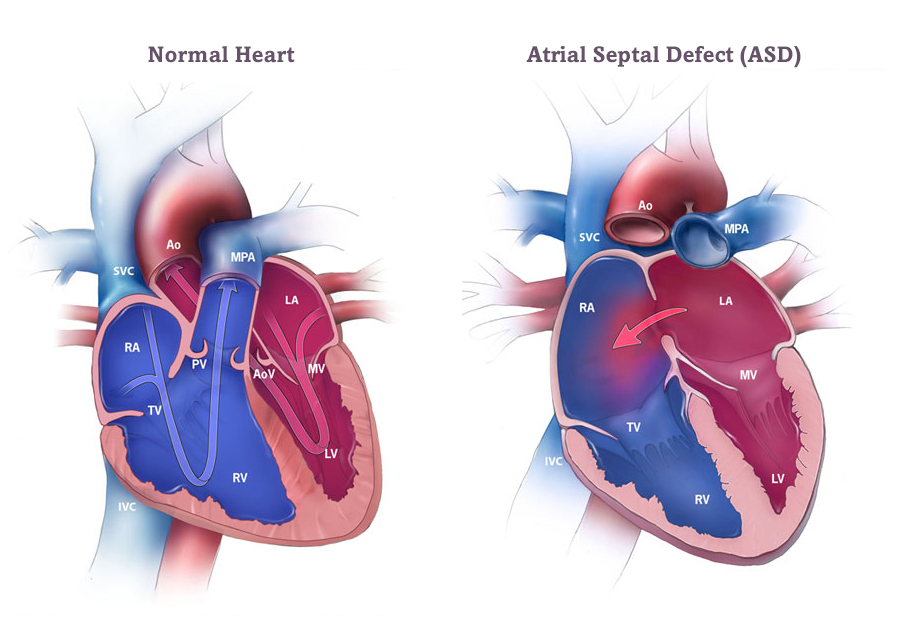
The aim of this trial was to assess the safety and effectiveness of the V-Wave Ventura Interatrial Shunt (IAS) device in symptomatic HF patients, regardless of LVEF, through a randomized, double-blind, placebo-controlled multicenter trial.
The trial screened 11,136 patients across 113 sites in 11 countries, ultimately enrolling 508 qualifying patients from 94 sites over a three-year period. Patients were stratified based on LVEF ≤40% or >40%.
The IAS device was successfully implanted in all patients without major procedural complications. Nearly all patients were discharged home the day after the procedure.
The trial concluded that the implantation of the V-Wave Ventura IAS device was safe but did not result in improvements in symptoms or prognosis for HF patients across the entire spectrum of LVEF - Comparison Of An “Inclisiran First” Strategy With Usual Care In Patients With Atherosclerotic Cardiovascular Disease:Results From The VICTORION-INITIATE Randomized Trial
The VICTORION-INITIATE trial aimed to assess the effectiveness of an “inclisiran first” strategy, which involves adding inclisiran to statins immediately if patients fail to reach LDL-C goals, compared to usual care in patients with ASCVD.
In this prospective trial, 450 patients were randomized 1:1 to receive either inclisiran plus usual care or usual care alone. Results showed that the “inclisiran first” strategy resulted in significantly greater reductions in LDL-C levels compared to usual care (60.0% vs. 7.0%).
Conclusions- LDL-C lowering with the “inclisiran first” strategy led to sustained LDL-C lowering, consistent with prior clinical studies of inclisiran.
- Most patients with ASCVD reached LDL-C goals at Day 330.
- Despite the study giving treating physicians access to LDL-C levels, and encouraging treatment according to lipid management guidelines, few patients in the usual care arm achieved guideline-recommended LDL-C goals.
- No new safety concerns were identified with twice-yearly inclisiran administration in a “real-world” clinical setting.
- Results from VICTORION-INITIATE demonstrate the clinical value of initiating inclisiran earlier in the treatment pathway and highlight the urgent need to improve usual care for patients with ASCVD.
- Once-weekly Semaglutide In Patients With Heart Failure With Preserved Ejection Fraction, Obesity And Type 2 Diabetes:Main Results From The STEP-HFpEF DM Trial
This presentation highlighted the effect of Semaglutide 2.4 mg once-weekly on function and symptoms in subjects with obesity-related HfpEF, and Type 2 Diabetes
A total of 616 participants underwent randomization. The mean change in the KCCQ-CSS was 13.7 points with semaglutide and 6.4 points with placebo (estimated difference, 7.3 points; 95% confidence interval [CI], 4.1 to 10.4; P<0.001), and the mean percentage change in body weight was −9.8% with semaglutide and −3.4% with placebo (estimated difference, −6.4 percentage points; 95% CI, −7.6 to −5.2; P<0.001).
The findings imply that semaglutide may offer disease-modifying benefits beyond weight loss, operating independently of weight reduction.
Best of ACC UpdatesBraunwald Heart Diseases 12th editioncardiacCardiac X-rays – V Chockalingamcardiocardio BloggercardiologyCardiomyopathieschest paindiseasesECGEndocarditisheartheart diseasePerloffs Clinical Recognition of Congenital heart diseaseRadiology and Imaging by Sutton 7th editionRadiology of Congenital heart disease by Kurt Amplatz