
Sodium glucose cotransporter-2 inhibitors and heart disease: Current perspectives
- SGLT2I IN PATIENTS WITH ASCVD
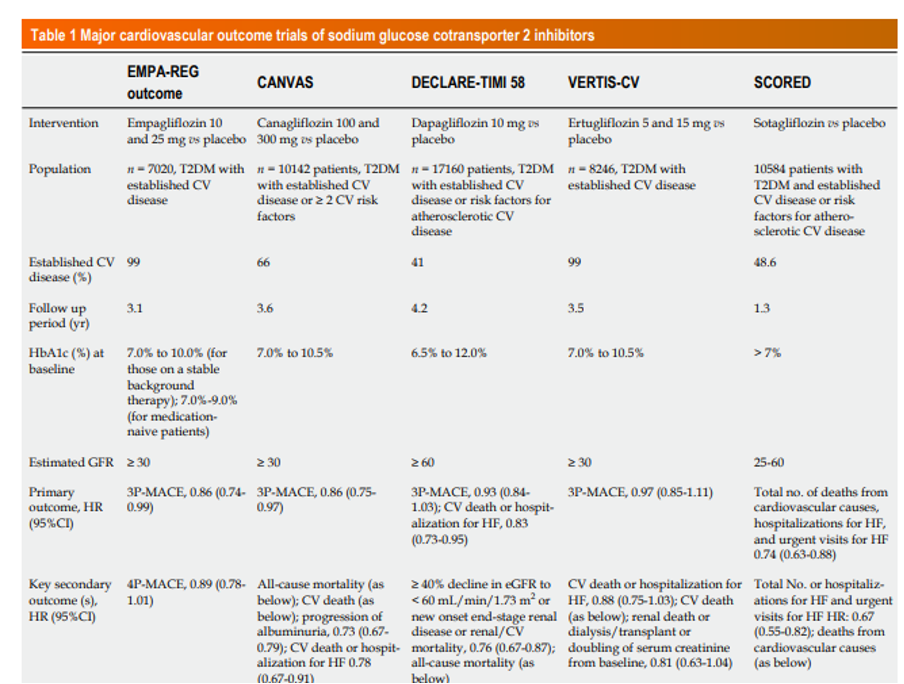
Cardiovascular outcome trials of SGLT2i in T2DM
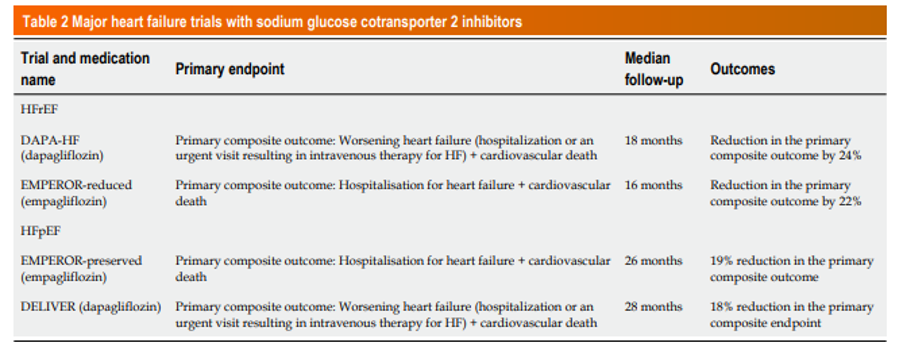
2. SGLT2I AND HEART FAILURE
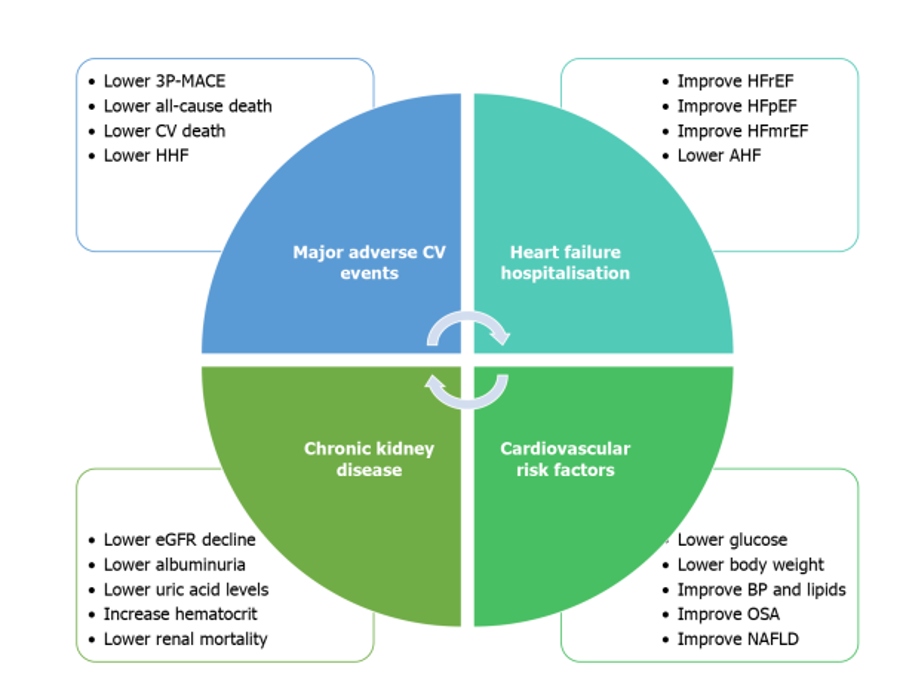
EFFECTS OF SGLT2I ON DIFFERENT CV RISK FACTORS
Effects on glucose levels | By inhibiting the SGLT2 cotransporters in the proximal convoluted tubules, they lower the blood glucose and have been found to reduce the HbA1c by around 0.5% in various trials |
Effects on body weight | 1. With the use of SGLT2i, there is a loss of glucose in the urine leading to the loss of calories which, in turn, results in the mobilisation of the fatty acids from the adipose tissue stores resulting in weight loss 2. In DAPA-HF, EMPERORReduced, and EMPEROR-Preserved trials, weight reduction of 0.9 kg, 0.8 kg, and 1.3 kg were observed respectively as compared to the placebo |
Effects on blood pressure | Because of the osmotic and diuretic effects of the SGLT2i, there is a modest reduction in blood pressure. In the DAPA-HF trial, there was a mean difference of around -1.4 mmHg in the systolic BP after 8 months which was significant when compared to the placebo |
Effect on lipid parameters | 1. there is a minor increase in LDL cholesterol with its use(SGLT2i might decrease the small dense LDL and increase the large buoyant LDL) 2. SGLT2i also resulted in an increase of high-density lipoprotein cholesterol by around 10%-11% 3. SGLT2i also decreases lipid deposition in the visceral fat, decreases lipid oxidation, and affect the transport of lipid into the cells |
Effects on albuminuria and progression of CKD | 1. SGLT2i can reduce intraglomerular pressure, and therefore albuminuria and also slow down GFR decline 2. SGLT2i can directly reduce oxidative stress, and angiotensinogen levels as well as reduce NLRP3 inflammasome activity in the kidney |
Effects on uric acid levels in serum | 1. The uricosuric effects of dapagliflozin, empagliflozin, and canagliflozin have been seen in patients with or without diabetes 2. The likely mechanism involves the GLUT9 isoform 2. By preventing reabsorption, SGLT2i can increase the concentration of glucose reaching the collecting ducts, which in turn compete with urate for reabsorption via the GLUT9 isoform 2 leading to the excretion of more uric acid 3. Other mechanisms involving activation of the xanthine oxidase by sirtuin activation and alteration of URAT1 transporter have been also proposed |
Effects on haematocrit | 1. All SGLT2i has been associated with a modest increase in haematocrit between 2%-4%. 2. SGLT2i can reduce metabolic stress and reduce ATP consumption by the Na+/K+ pump, causing a possible reversion of myofibroblasts to erythropoietin-producing fibroblasts and elevation of the haematocrit 3. Additionally, the nephroprotective effect of SGLT2i which prevents progression of CKD can also improve erythropoietin levels. |
Effects on inflammatory markers | 1. Reduced IL-1β, IL-6 and IL-10 levels have been seen with empagliflozin, while dapagliflozin has demonstrated reduced NLRP3, IL-1β and IL-18 levels |
Effects on metabolic syndrome-associated fatty liver disease | 1. SGLT2i can lead to reduction in the de-novo lipid synthesis in the liver 2. the glucagon-secreting alpha cells express SGLT2, and inhibition of this reduces intracellular glucose concentration in them thus increasing the secretion of glucagon 3. The high glucagon levels and elevated glucagon/insulin ratio can stimulate β-oxidation leading to a shift from carbohydrate to fatty acid metabolism and reduction in the hepatic triglyceride content 4. Canagliflozin has been found to significantly reduce FIB-4 index and ferritin levels in T2DM patients with MAFLD, suggesting improvement in hepatic fibrosis 5. Dapagliflozin has also been shown to reduce Fibroblast Growth Factor 21 levels and indices of hepatocyte injury |
Effects on obstructive sleep apnea | 1. SGLT2i have been found to reduce apnea-hypopnea index in patients with T2DM with OSAS in small studies 2. Postulated beneficial mechanisms could include rostral nasal fluid shift due to diuresis and reduction of circadian sympathetic nerve activity, nocturnal hypertension, and oxidative stress by which SGLT2i might reduce the incidence or the CV effects of OSA |
CARDIOVASCULAR BENEFITS WITH SGLT2I – POSSIBLE MECHANISMS
SGLT2I – DIRECT EFFECTS ON MYOCARDIUM AND BLOOD VESSELS

CAUTION AND CONTRAINDICATIONS TO THE USE OF SGLT2I IN HEART DISEASE
- The glucosuric effect of SGLT2i leads to higher urine glucose levels and thus predisposes patients to urinary tract and genital infections. In the large three CVOT outcome trials, the rates of UTI were not significantly increased when compared with placebo. Available real-world data highlight the fact that SGLT2i do not increase the frequency of UTIs compared to either DPP 4 inhibitors or GLP1 receptor agonists. However, genital mycotic infections have been consistently found to be more frequent in patients on SGLT2i in all three major CVOT outcome trials. Risk factors for genital mycotic infection include female gender and previous history of genital infection.
- SGLT2i have an osmotic diuretic effect, thus a mild volume depletion state can be observed with them. A slight reduction in blood pressure, orthostatic hypotension, and dizziness can occur with these agents especially when combined with diuretics. it is recommended to review the dose of diuretics while initiating a patient with SGLT2i to prevent postural hypotension.
- The use of SGLT2i is associated with increased circulating ketone bodies. The incidence of euglycemic diabetic ketoacidosis varies from study to study. CANVAS and EMPAREG trials reported a nonsignificant increase of euglycemic DKA, but DECLARE-TIMI 58 reported a small but significant increase of the same. Real-world data however suggests slightly higher rates of DKA among SGLT2i users. Risk factors for euglycemic DKA included T1DM, presence of dehydration, excess alcohol intake, critical illness, post-operative period and intake of very lowcarbohydrate die
- The FDA had issued a warning for AKI with dapagliflozin and canagliflozin in 2016 based on few case reports submitted to the FDA adverse events reporting system (FARES). The possible mechanisms that mediate renal damage by SGLT2i could be related to volume depletion by osmotic diuresis, decreased trans glomerular pressure, and hypoxic injury to the renal medulla. The real-world data also suggest the use of SGLT2i is not associated with an increased risk for AKI.
- There was a postulation that SGLT2i may affect bone mineral density and bone quality, thereby increasing the risk for fragility fractures. Initial studies with canagliflozin reported a mild increase in serum phosphate, parathyroid hormone, bone resorption markers, and bone formation markers and a slight reduction in total hip bone mineral density without affecting the rest of the skeleton. The underlying mechanism for increased incidence of fracture with canagliflozin can be a direct effect on bone metabolism, or it can be due to an increased risk for falls due to orthostatic hypertension associated with SGLT2i.
- An increased incidence of lower limb amputations was seen with canagliflozin compared to placebo (6.3 vs 3.4 participants with amputation per 1000 patient-years) in CANVAS trial, but not with other SGLT2i.
- A concern regarding an increase in bladder malignancies in male patients receiving dapagliflozin was raised in initial studies. Possible mechanisms for tumor genesis with an SGLT2i could be the enhanced tumor growth from bladder epithelium due to persistent glycosuria in as well as the effects of chronic cystitis or recurrent urinary tract infections.







