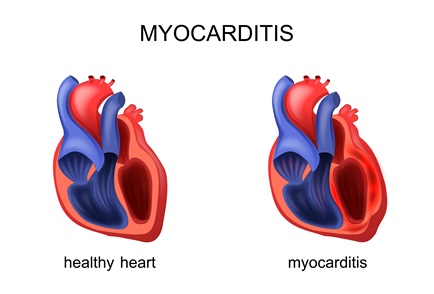
The following are key points to remember from a 2024 American College of Cardiology (ACC) expert consensus decision pathway (ECDP) on strategies and criteria for the diagnosis and management of myocarditis:
© 2022 Cardio Blogger. All Right Reserved | Designed & Developed By Diviants