Clinical Update on Myocardial Infarction With No Obstructive Coronary Artery Disease (MINOCA)
18 June 2024

Clinical Update on Myocardial Infarction With No Obstructive Coronary Artery Disease (MINOCA)
Canadian Cardiovascular Society/Canadian Women’s Heart Health Alliance
Definition
MINOCA is defined as MI (per the fourth Universal Definition of MI) without significant coronary artery stenosis (ie, > 50%) on coronary angiography.
- Meets criteria for AMI, per fourth universal definition of myocardial infarction; detection of an increase and/or decrease in troponin level with at least 1 value > 99th percentile
And at least 1 of the following:
- Symptoms of myocardial ischemia
- New ischemic ECG changes
- Development of pathological Q waves
- Imaging evidence of new loss of viable myocardium or new RWMA consistent with ischemic etiology
- Identification of a coronary thrombus using angiography or in autopsy
- No obstructive coronary artery disease ( 50% stenosis) in any epicardial artery or overlooked form of obstructive disease (spontaneous coronary artery dissection, embolus)
- No clinically overt specific cause for the acute presentation (ie, myocarditis, Takotsubo cardiomyopathy)
Epidemiology
- The reported incidence of MINOCA is variable, representing up to 15% of MIs, with the largest cohort studies reporting that MINOCA represents 6% of all MIs
- In the largest meta-analysis of 28 studies (median patient age 55 years; 40% female), a comparison of patients who presented with MI caused by obstructive CAD (MI-CAD) showed MINOCA patients to be younger, twice as likely to be female, and less likely to have hyperlipidemia, although other cardiovascular risk factors were similarly prevalent
- In the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, MINOCA was seen in 1 of 8 women younger than the age of 55 years who had an acute MI, and these younger women had fivefold greater odds of MINOCA compared with young men who presented with an acute MI
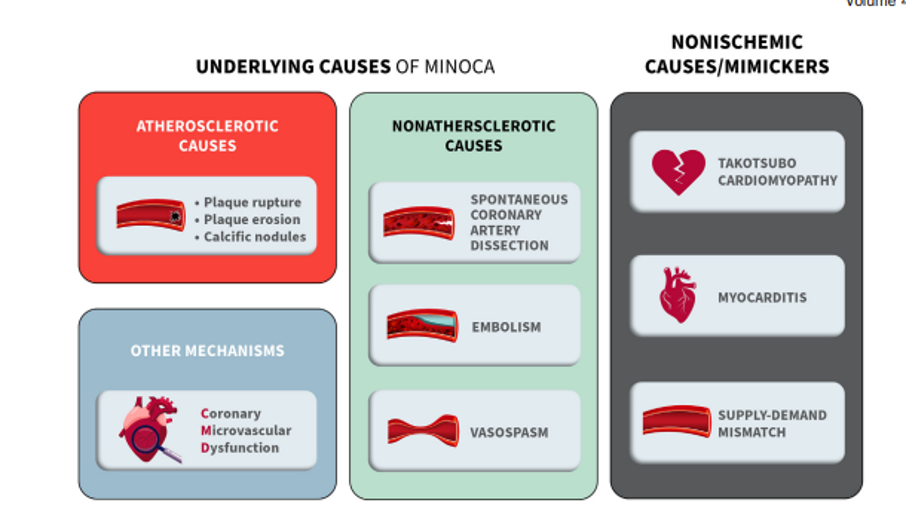
Pathophysiology of MINOCA
Clinical Presentation
- Patients with MINOCA usually present similarly to patients with MI-CAD, with symptoms characterized most often by acute chest discomfort or dyspnea, and elevated cardiac troponin level
- MINOCA occurs more frequently in the setting of a non-ST elevation MI compared with STelevation MI (STEMI).
Prognosis
- The prognosis of patients who present with MINOCA is not benign. major adverse cardiovascular events (MACEs), and readmission rates has been reported to be similar or lower, but not insignificant, for all age groups of patients with MINOCA compared with those with MI-CAD
- In a large single-centre contemporary analysis, the composite rate of mortality or nonfatal MI associated with MINOCA was more than twice that for patients without previous atherosclerotic cardiovascular disease (4.6% vs 2.2%), and compared with those with MI-CAD, it was approximately one-third (4.6% vs 14.3%)
- In a recent publication including 8560 consecutive STEMI patients, 5-year mortality hazard risk was 1.93 times higher in patients with MINOCA than those with MI-CAD
Investigations and Diagnosis
Practical tips: MINOCA diagnosis
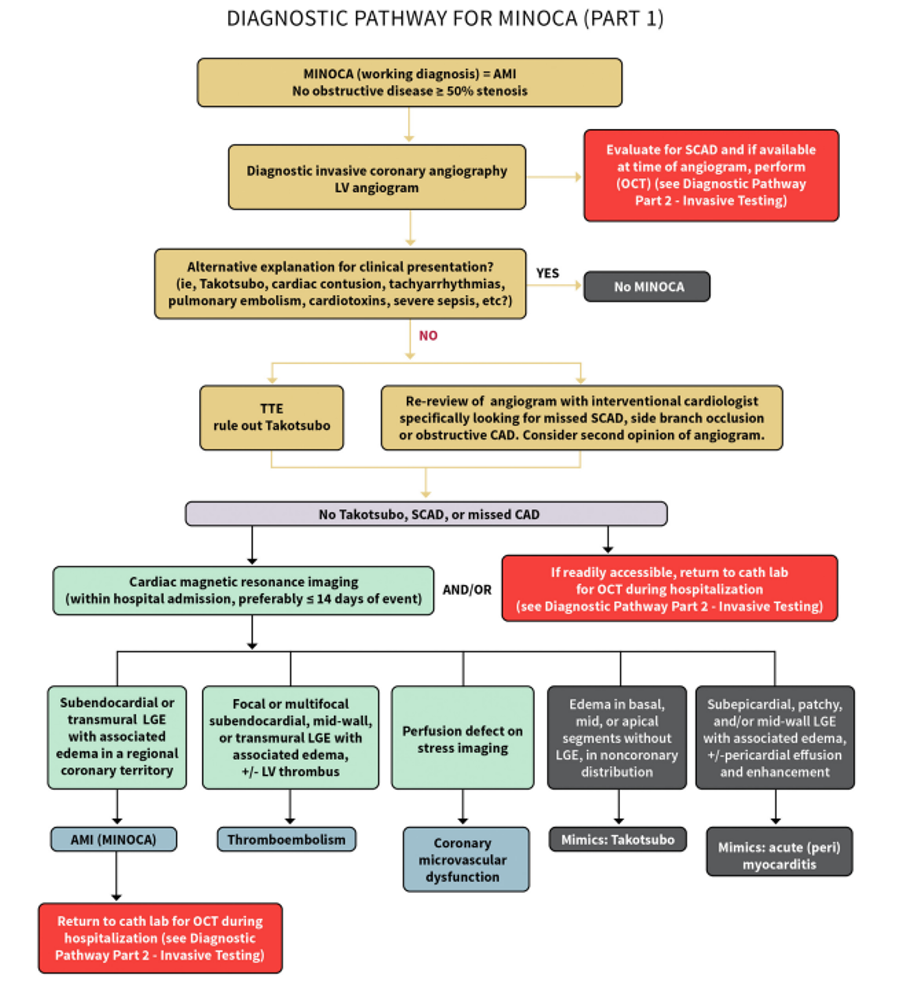
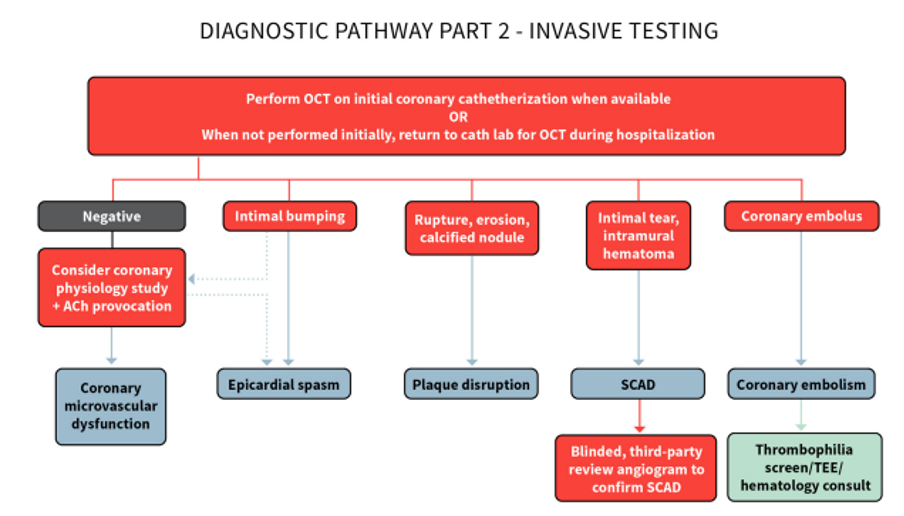
- Clinicians are encouraged to follow a cascaded approach in which the first step is to make a working diagnosis of MINOCA; then exclude SCAD, small-branch coronary occlusions, and mimickers (ie, Takotsubo, myocarditis); and then chose a diagnostic path that best suits their clinical setting (early noninvasive path starting with CMR; or an early invasive path starting with intracoronary imaging).
- Echocardiography is uniformly recommended in all patients regardless of the diagnostic path chosen, because of its wide availability, low risk, relatively low cost, and significance of the information gained from this test (such as identification of RWMAs, or diagnosis of mimicker diagnoses such as Takotsubo or underlying cardiomyopathy).
- When an early noninvasive path is chosen, we recommend performing CMR within 1-14 days of presentation, and as early as possible, so as not to miss a potential diagnostic window for small infarcts, Takotsubo, or mild myocarditis.
- When an early invasive path is chosen, clinicians might adapt to the workflow of their catheterization laboratory to decide whether to perform intracoronary imaging at the time of index coronary angiography, or during a subsequent return to the catheterization lab after alternative diagnoses have been excluded.
- CMR and intracoronary imaging are considered firstline tests for MINOCA diagnosis. When CMR and intracoronary imaging (OCT) are performed, the etiology of MINOCA can be successfully identified in 85% of patients, which significantly aids in treatment and prognosis.
- Diagnostic tests such as cardiac PET, coronary computed tomography angiography, invasive coronary provocative testing, and thrombophilia workup are considered supplementary tests to be used on the basis of case-by-case indications
Treatment of MINOCA
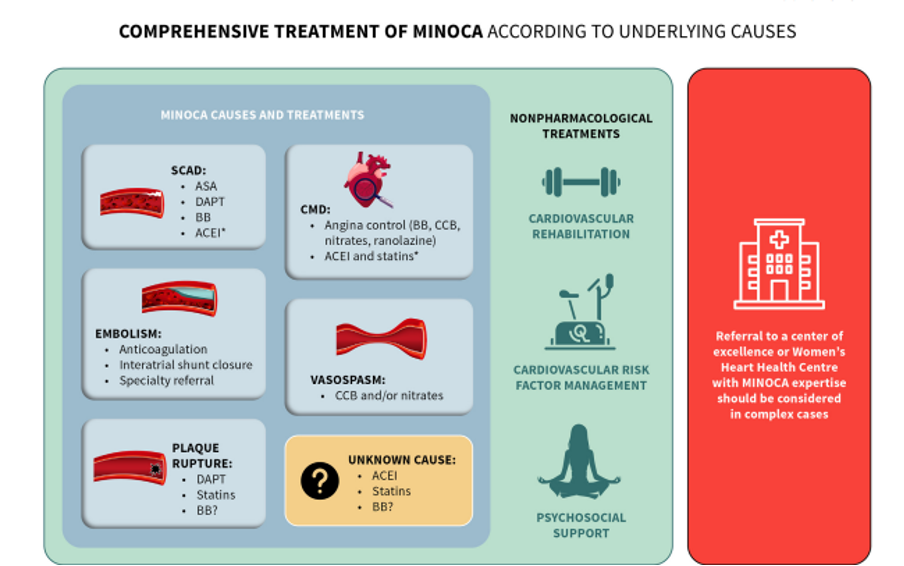

Practical tips: Cause-specific treatment of MINOCA
- MINOCA in the context of confirmed plaque disruption should be managed similarly to obstructive CAD.
- Antianginals including b-blockers, CCB, nitrates, and ranolazine should be considered for chest pain and quality of life in patients with MINOCA secondary to CMD. ACEIs and statins should be considered for CMD patients in whom there is already an indication.
- CCB (often dual pathway) and/or nitrates should be considered for patients with MINOCA from vasospasm.
- Aspirin and b-blockers are the mainstay medications for patients with SCAD and should be strongly considered.
Practical tips: MINOCA of unknown underlying cause
- ACEI/ARB therapy should be considered in patients with MINOCA from plaque disruption or in whom an obvious other cause has not been identified.
- Statins should be considered in all patients in whom a specific cause has not been identified, considering potential event and mortality benefit with minimal risk.
- There is a lack of evidence to support the use of b-blockers in the absence of another indication.
- There is currently little evidence that supports the systematic use of DAPT in the context of MINOCA. The decision to use DAPT should be made in view of the most likely underlying diagnosis.







