Cyanosis in Heart Disease
A. Definition
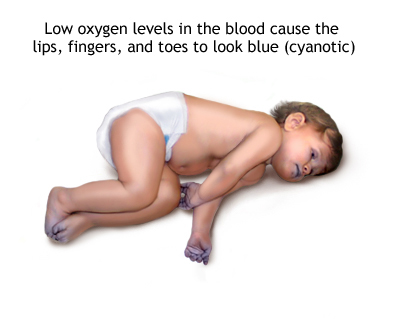
Cyanosis is a bluish discoloration of the skin and mucous membrane resulting from an increased quantity of reduced hemoglobin or of abnormal hemoglobin pigments in the blood perfusing these areas.
B. Types of Cyanosis
(i) Central Cyanosis
Central Cyanosis is due to arterial blood unsaturation or an abnormal Hb derivative with the mucous membrane and skin both being affected. Central cyanosis is seen in
1) R-L Shunt(Congenital heart disease)
2) Impaired pulmonary function
3) Abnormal hemoglobin
(ii) Peripheral Cyanosis
Peripheral cyanosis is secondary to cutaneous vasoconstriction due to a) low cardiac output b)exposure to cold air or water causing slowing of blood flow and an abnormally greater extraction of oxygen from normally saturated blood. It is seen in
1) Decreased cardiac output
2) Cold exposure
3) Redistribution of blood flow
4) Arterial obstruction
5) Venous obstruction
| Central Cyanosis | Peripheral Cyanosis |
| O2 saturation is < 85% | O2 saturation is normal |
| Arterial blood unsaturation | Increased peripheral utilization |
| Skin & mucous membrane involved | Skin only is involved |
| Skin over cyanosis is warm | Skin over cyanosis is cold & clammy |
| Clubbing | No clubbing |
| Polycythemia | No Polycythemia |
| O2 therapy has no effect | O2 therapy improves |
| Warming – No effect | Warming – Improves |
| Exercise – worsens | Exercise – improves |
| AV O2 difference is normal – 5 vol% | AV O2 diff is greater >12 vol% |
| P O2 is decreased | PO2 is normal |
Only 2 congenital heart disease where oxygenation increases O2 saturation are
1) TAPVC
2) Pulmonary AV fistula
C. Causes
(i) Congenital heart disease
(ii) Pulmonary A-V Fistula
(iii)Multiple small intrapulmonary shunts
(iv) HEMOGLOBIN ABNORMALITIES
a. Methemoglobinemia
b. Sulfhaemoglobinemia
c. Carboxyhaemoglobinemia
D. Sites Of Cyanosis
1) Lips 5)Cheeks
2) Ear lobes 6)Hand and feet
3) Nose tip 7) Finger tips
4) Nail bed 8) Trunk
Cyanosis is better observed in hands and feet because 1) skin is thin 2) Skin is unpigmented and 3) capillaries are numerous. Cyanosis is rarely seen in trunks because there is not enough blood vessels in the skin.
E. Cyanotic Point
1) O2 saturation < 85%
2) Deoxyhaemoglobin > 5 gm/100 ml
3) Methaemoglobin > 2 gm/100 ml
4) Sulphaemoglobin > 0.5 gm/100 ml
5) O2 unsaturation > 6.5 vol%
6) R-L shunt > 25% of LV output.
F. Cyanosis Overlooked
1) Anaemia (Hb < 33% of normal)
2) Secondary Polycythemia (Not yet developed)
3) Arterial Blood O2 saturation (85-93%)
4) Increased skin pigmentation
5) R-L shunt < 40%
6) Blood shunted away from skin
G. Types of Cyanosis
(i) Differential Cyanosis
Presence of differential cyanosis in a patient indicates
1) Presence of a congenital heart disease
2) Patency of ductus arteriosus.
If not obvious clinically differential cyanosis can be provoked by
1) exercise
2) Warming the hand and feet (Which increases skin blood flow)
Confirmation – Simultaneous O2 saturation in femoral and brachial artery
Upper Part Pink Lower Part Blue
1) PDA with reversal of shunt
2) Coarctation of aorta with PDA and reversal of shunt
3) Interruption of Aortic arch with PDA and reversal of shunt
4) Tubular hypoplasia of Aortic arch with PDA and reversal of shunt
Right Arm Pink Left Arm Blue Lower Part Blue
1) If unoxygenated blood enters the left subclavian artery
2) If ductus arises from Left Subclavian artery
Right Arm Blue Left Arm Pink Lower Part Blue
1) Right sided ductus
2) Aberrant Rt subclavian distal to the ductus.
(ii) Reversed differential cyanosis
1. Transposition of great Vessels with Co of aorta with PDA with reversal of shunt
Oxygenated blood –> Pulmonary veins–>LA–> LV–>PT–> Ao–>Supplies lower half of body
2. Taussing Bing anomaly
DORV with Subpulmonic VSD with PDA with reversal of shunt
Oxygenated blood–> PV–> LA–> LV–> VSD–> Into PA–> PDA–> Aorta–> Lower
limbs. RV blood enters aortic root and supplies upper half.
(iii) Deffered Cyanosis
In deferred cyanosis the child is not cyanotic at birth but after 3-6 months the child becomes cyanotic and thereafter the cyanosis is persistent. Causes are
1) Persistence of ductal patency
2) Persistence of fetal hemoglobin
3) Decreased energy expenditure at birth
4) Progressive infundibular stenosis
Deferred cyanosis is seen in TOF and TOF physiologies-
1) Tetralogy of Fallot
2) L-TGV VSD with PS
3) DORV VSD with PS
4) SV VSD with PS
5) TGV VSD with PS
(iv)Transient Cyanosis
In Transient cyanosis the child is born at birth with cyanosis and after a month when the PVR falls the cyanosis regresses. The cyanosis is due to R-L shunt caused by the increased PVR, which ceases when the PVR comes down. It occurs in
1) ASD
2) Ebsteins anomaly
3) DORV with subaortic VSD without PS.
4) Truncus arteriosus
(v) Intermittent Cyanosis
Intermittent cyanosis occurs in these conditions where strain, exercise or arrhythmia brings out a transient R-L shunt and cyanosis. Causes are
1) Ebsteins anomaly
2) TAPVC unobstructed
3) Complete A-V canal defect
4) Eisenmengers with bidirectional shunt
(vi) Persistent Cyanosis
Persistent cyanosis appears at birth and after that it remains persistent and is either static or progressive.
It occurs in
1) Transposition of great vessels
2) Single ventricle
3) Hypoplastic Left Heart syndrome
4) Tricuspid atresia
5) Pulmonary atresia
6) Ebsteins anomaly
Ebsteins anomaly is one condition which can have all the three types of cyanosis a)Transient b) Intermittent and c)Persistent.
(vii) Cyanosis Tardive
Cyanosis tardive or very late onset cyanosis is cyanosis which occurs after first decade due to reversal of L-R shunt as seen in
1)Eisenmenger syndrome due to pre and post tricuspid shunts
2) Triology of Fallot ( PS with R-L shunt at PFO)
H. Factors affecting Cyanosis
1) Skin pigmentation
2) Amount of haemoglobin
3) Amount of deoxygenated haemoglobin
4) Colour of blood plasma
5) Skin thickness
6) Capillary density
7) Capillary orientation
8) Vessel caliber
I. Approach To Cyanotic Heart Disease
The following issues should be looked into in a patient with cyanotic heart disease to get clues that will lead us to the diagnosis
1) History of exposure to drugs?
2) Type of cyanosis?
3) Cyanosis with failure
4) Cyanosis with squatting
5) Differential cyanosis
6) Reversed differential cyanosis
7) Cyanosis with a wave in JVP
8) Cyanosis with Collapsing pulse
9) Cyanosis with continuous murmur
10) Cyanosis with LAD in ECG
11) Cyanosis with LV/RV/Combined apical impulse
PS: Approach will be discussed later.