Lipid Association of India 2023 update on cardiovascular risk assessment and lipid management in Indian patients: Key Points
12 August 2024
Lipid Association of India 2023 update on cardiovascular risk assessment and lipid management in Indian patients: Key Points
- The previous LAI recommendations have found increasing acceptance among various national and international lipid experts and clinicians in India. The current recommendations provide updated guidance for ASCVD risk estimation in Indians based on expert opinion and the latest scientific data.
- Family history of premature ASCVD (defined as occurrence of an ASCVD event in a male first-degree relative <55 years of age and in a female first-degree relative <65 years of age or before menopause) identifies individuals at an elevated ASCVD risk. In the current algorithm, a family history of premature ASCVD has been designated as a high-risk feature for estimation of ASCVD risk
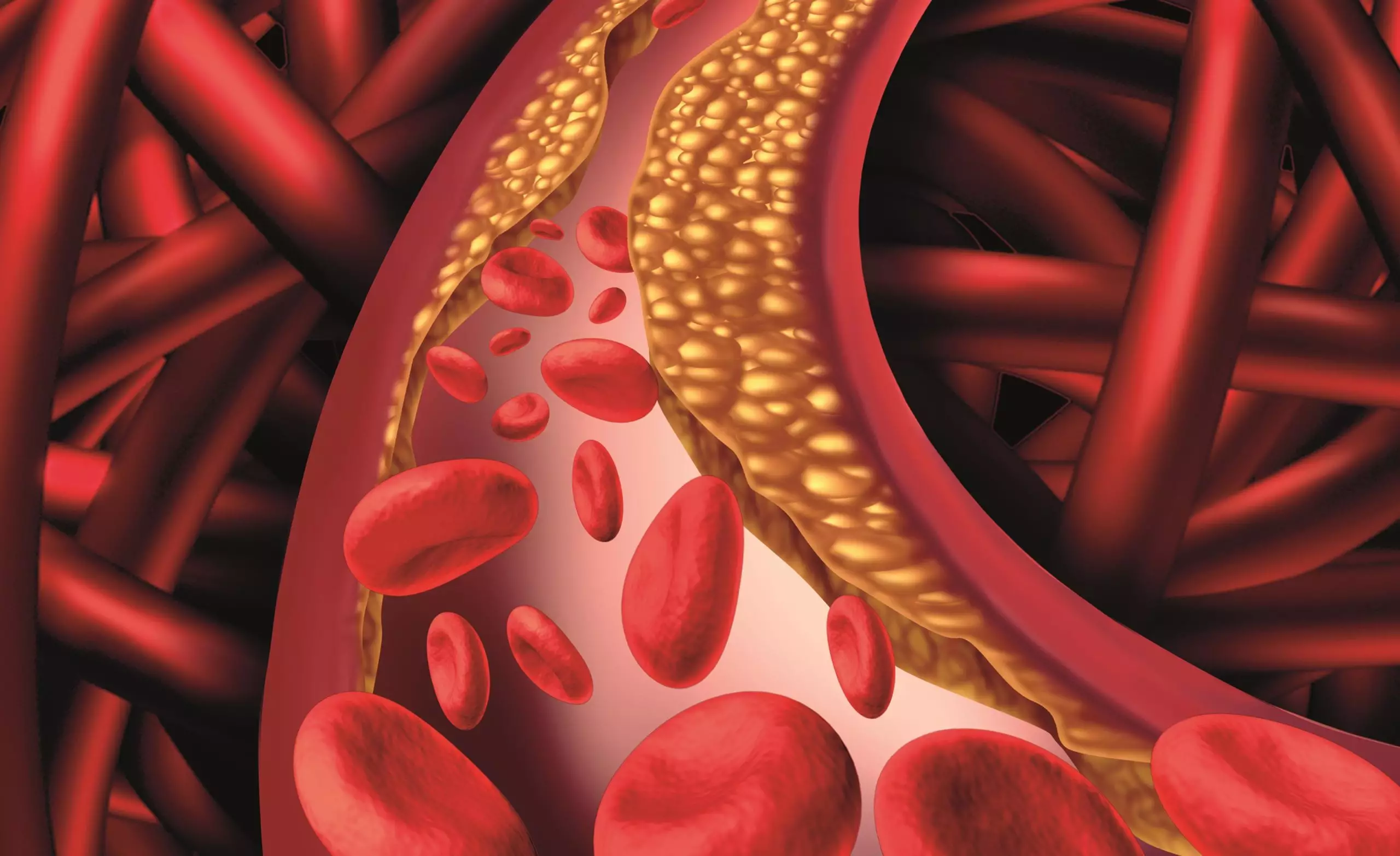
- Assessment for subclinical ASCVD reflects the cumulative effects of all known and unknown ASCVD risk factors as well as the individual susceptibility to develop the disease, thereby providing a more robust prediction of future ASCVD risk than the traditional risk assessment models.
- CACS is an excellent predictor of incident ASCVD events, and the predictive power is incremental to any conventional risk factors and risk algorithms for primary prevention. Patients with CACS values ≥100 have 10-year ASCVD event rates in the range of 10-15%.In contrast, zero CACS is associated with a very low risk of events over the subsequent 5-10 years, except in individuals who have multiple ASCVD risk factors with high ASCVD risk as determined by the clinical risk scores.
- In addition to lipid-lowering therapy, other evidence-based therapies for cardiovascular risk reduction (e.g. low dose aspirin) are recommended in patients with CACS ≥100. In subjects with CACS 1-99, antiplatelets may be required based on presence of associated ASCVD risk factors, comorbidities and physician clinical judgement.
- Several studies have demonstrated that the presence of lumen encroaching, but hemodynamically non-obstructive carotid or femoral plaques is associated with a high risk of cardiovascular events. Plaque assessment has also been shown to be more informative than the measurement of carotid intima-media thickness. Thus, the available evidence suggests that assessment of carotid and femoral arterial plaque burden may be a useful tool for ASCVD risk prediction
- The 2016 LAI recommendations designated ABI <0.9 as evidence of established ASCVD, with LDL-C targets similar those for patients with ASCVD
- Assessment for subclinical atherosclerosis is recommended for persons aged 30 years and over for whom treatment decisions may be uncertain after consideration of risk scoring and additional risk factors and high-risk features, especially in the following scenarios:
- Individuals considered to be in the moderate risk and high risk group as per the LAI risk algorithm
- Family history of premature ASCVD or uncertain family history
- Suspected or diagnosed familial hypercholesterolemia (FH)
- Individuals with multiple ASCVD risk factors
- Individuals with reluctance for or intolerance to statin therapy
- NAFLD has also been demonstrated to be an independent risk factor for ASCVD. Patients with NAFLD have increased ASCVD risk as compared to those who have same risk factors without NAFLD. In view of the close association between NAFLD and ASCVD risk factors, and recognition that ASCVD is the leading cause of death in patients with NAFLD, the LAI designates NAFLD with fibrosis grade 2 or 3 as a high-risk feature. The presence of NAFLD would require an LDL-C goal <50-70 mg/dL, depending on the overall risk profile of the patient.
- LAI proposes designation of the metabolic syndrome as a high-risk feature with risk proportional to the number and severity of the metabolic syndrome factors present. The presence of metabolic syndrome would require an LDL-C goal <50-70 mg/dL, depending on the patient’s overall risk profile.
- Several female specific ASCVD risk enhancing factors have been identified. Premature menopause is one condition that is associated with increased risk of ASCVD. Several pregnancy-associated complications are also associated with increased risk of ASCVD during later life. PCOS is associated with higher triglycerides, higher total cholesterol and lower HDL-C
- Rheumatoid arthritis (RA) and spondyloarthropathies (e.g., ankylosing spondylitis and psoriatic arthritis) are associated with significantly increased ASCVD risk.
- “Targets of lipid-lowering therapy will continue to be LDL-C, non-HDL-C, and Apo-B, [and potentially lipoprotein(a) when specific therapies become available], with the awareness that hypertriglyceridemia is a marker for persistent ASCVD risk”. The expert panel has designated plasma triglycerides ≥150 mg/dL fasting or ≥175 mg/dL non-fasting as a risk modifier in the treatment algorithm.
- Genetic predisposition for development of ASCVD is an important modulator of interindividual ASCVD risk, as well as the atherogenic response to individual risk factors. PRS(Polygenic risk score) may have greater relevance for Indians because of higher incidence of premature ASCVD as compared to Western populations.
- Infection with human immunodeficiency virus (HIV) increases ASCVD risk through several mechanisms. Active inflammation, prolonged activation of the immune system, long-term use of anti-retroviral therapy, Endothelial dysfunction, concomitant infection with hepatitis C are proposed mechanisms.
- Exposure to air pollution should at least be considered a risk modifier in the clinician-patient discussion about ASCVD risk assessment and identification of optimum LDL-C targets.
cardiaccardiocardio BloggercardiologyCardiomyopathycardiovascular riskcardiovascular risk assessmentchest paindiseasesECGheartheart diseaseLipid AssociationLipid Association of IndiaLipid Association of India 2023 update on cardiovascular risk assessment and lipid management in Indian patientslipid managementlipid management in Indian patients