A. General Rules
1)Bundle Branch Block Pattern
•RBBB(LV)
•LBBB(RV/IVS)
2)QRS Axis
•Superior/Inferior (Lead II/III)
•Right/Left (Lead I/aVR & aVL)
3)Precordial Transition
•RBBB PVC: Progressively earlier as SOO moves from base toward apex
•LBBB PVC: Progressively later as SOO moves from septum towards RV free wall
4)QRS width:
•Narrow: Septal/Wide: Free wall


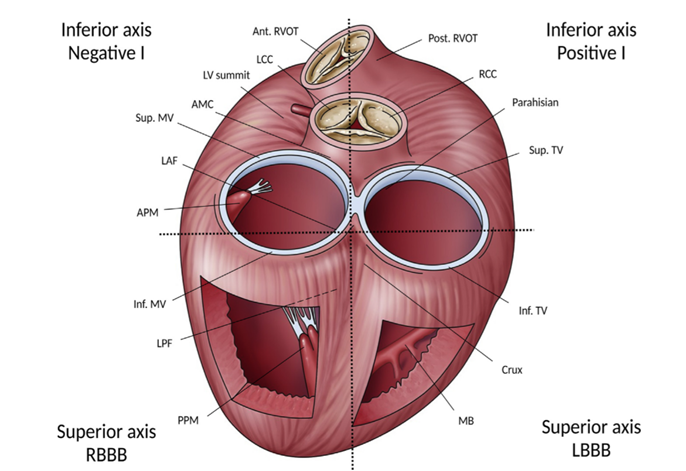
B. Step wise approach for PVC
Step 1: Superior/Inferior Axis (Lead II/III)
• Inferior Axis (+ve II/III): Basal areas of heart, outflow tract, superior aspect of MV/TV
•Superior Axis (-ve II/III): Inferior aspect of both ventricles
•Inferior lead discordance (+ve II/-ve III or –ve II/+ve III): midcavitary structures
Step 2:
•Inferior axis PVC: Lead I
+ve I: rightward structures (posterior RVOT, RCC, Parahisian, superior aspect of TV)
-ve I: leftward structures (anterior RVOT, LCC, AMC, AL-MA, LV summit)
Midline structures like RCC-LCC commissure can have +/- or biphasic I.
•Superior axis PVC: BBB pattern
LBBB: inferior TV, Moderator band, Cardiac Crux
RBBB: inferior MV, Posterior PM, left posterior fascicle
Step 1 & 2 localizes SOO to one of these four quadrants

Step 3:
•More refined localization
•Specific ECG characteristics

Example 1

Example 2

Example 3

C. PVC – Clinical Scenarios
I.Common clinical scenario:
ARIC study – 5.5%(2 minute ECG)
Framingham heart study – 12%(1 hour ECG)
Population study, Lichtenstein – 69% (24 hour ECG) median 2 PVC
II. In the absence of structural/electrical heart disease (H+P, ECG, Echo) “Benign” condition with excellent long term prognosis
III. Yearly examination and evaluation of LV function (high burden PVCs)
2. Symptoms
•Pounding ‘Extra Beat’ – Post PVC beat
•‘Skipped Beat’ – Post PVC Pause
•Effort intolerance, Fatigue, Tiredness, Shortness of Breath – Concealed Mechanical Bradycardia, Retrograde VA
•Syncope – Detailed evaluation….
3. Cardiomyopathy
•Important to differentiate PVC induced cardiomyopathy from PVC in cardiomyopathy. •PVC induced cardiomyopathy:
1.Frequent PVC – High burden PVC
2.LV dilatation and reduced LV function
3.Reversible with PVC elimination
It is not a form of tachy-cardiomyopathy. Frequently asymptomatic or minimal symptomatic.
Risk factors for PVC induced cardiomyopathy
1.PVC Burden: cut-off of 24% sensitivity of 79% and specificity of 78% for prediction of PVC cardiomyopathy
2. PVC Duration & Asymptomatic status:
3. QRS Duration & PVC location:
•Wide>Narrow, Epi>Endo, RV>LV
4. Others:
•Male
•Lack of diurnal variation in PVC frequency
•Interpolated PVCs
•Nonperfused PVCs
•Lack of post PVC potentiation
Predictors of CMR abnormality in apparently ‘idiopathic PVC’
I.History – Syncope
II.ECG -Abnormal Baseline ECG
III.TMT – Exercise induced VT
IV.Holter – Multiple Morphologies, Evidence of AV conduction disease

4. Cardiac arrest
•1139 CHS participants
•Randomly assigned to 24 hour Holter, Normal LVEF, No CHF
•PVC frequency & LVEF at baseline and 5-years.
•Followed for incident CHF and death
•Conclusion:
1.An increased percentage of PVCs was associated with a subsequent decrease in the LVEF, increased incident CHF, and increased mortality.
2.Increased mortality appeared to be at least partly mediated by incident CHF
3.The risk of incident CHF attributable to PVCs was comparable to that of other CHF risk factors


PVC as a trigger of VF (IVF)

D. Risk Stratification
Proposed flow chart for the diagnostic work up and management of patients presenting with
apparently idiopathic PVCs

E. Treatment



© 2022 Cardio Blogger. All Right Reserved | Designed & Developed By Diviants