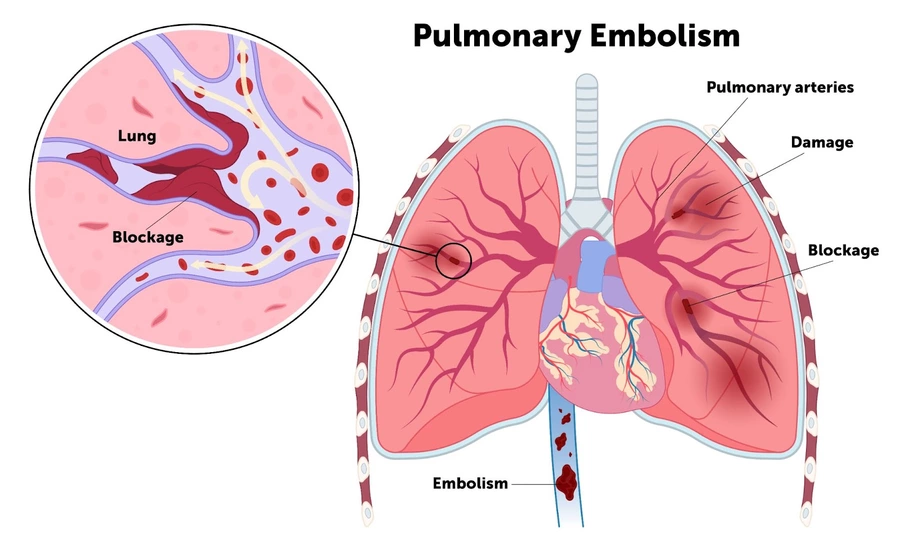
Pulmonary Embolism Guideline Comparison: Key Points
The following are key points to remember from a review comparing international clinical practice guideline recommendations for acute pulmonary embolism (PE):
- This review compared guidelines and other society recommendations from the European Society of Cardiology and European Respiratory Society (ESC/ERS), Pulmonary Embolism Response Team consortium (PERT), American College of Chest Physicians (CHEST), American Heart Association (AHA), American Society of Hematology (ASH), and National Institutes for Health and Care Excellence (NICE).
- Most current guidelines emphasize initial patient assessment using validated pretest probability scores, such as the Wells’ or Geneva scores. All recommend D-dimer testing to exclude acute PE in non–high pretest probability cases. ESC/ERS and PERT suggest using an age-adjusted or probability-adapted D-dimer cutoff. NICE and ASH suggest using age-adjusted cutoff for patients aged >50 years. ASH, NICE, and PERT suggest using the PE Rule-out Criteria (PERC) in patients with low pretest probability. ESC/ERS does not incorporate PERC criteria, noting that the evidence for its use is limited.
- There is variation in imaging recommendations for diagnosis. ESC/ERS, NICE, and PERT recommend computed tomographic pulmonary angiography (CTPA) as first-line for acute PE diagnosis. ASH recommends using ventilation/perfusion (V/Q) lung scans over CTPA to reduce radiation exposure when this can be done rapidly and interpreted expertly.
- During pregnancy, ESC/ERS guidelines assert that the diagnosis of PE should be considered in the presence of high pretest probability (Geneva score) or intermediate/low probability with a positive D-dimer test. They recommend CTPA for further diagnosis imaging, using a low-dose radiation protocol. ESC/ERS guidelines suggest the use of customized strategies, such as a modified YEARS algorithm, to limit the use of CTPAs. ASH suggests using V/Q scanning as the primary imaging modality in pregnant patients being evaluated for acute PE.
- To diagnose right ventricular (RV) dysfunction, the ESC/ERS guidelines suggest use of a comprehensive echocardiogram with RV/left ventricular (RV/LV) diameter ratio of ≥1.0 and tricuspid annular plane systolic excursion (TAPSE) of <16 mm. They also suggest using a CTPA RV/LV ≥1.0 to define RV dysfunction. The AHA has similar RV/LV ratio criteria for both echocardiography and CTPA, while the PERT document does not endorse specific definitions. CHEST, ASH, and NICE do not provide specific recommendations for assessment of RV dysfunction.
- The use of validated prognostic scores (e.g., PE Severity Index [PESI], simplified PESI) is endorsed by ESC/ERS, PERT, and ASH. ESC/ERS and CHEST also recommend assessing RV size and function to identify low-risk patients with acute PE.
- AHA and ASH recommend diagnosing intermediate-risk PE when RV dysfunction or strain are detected, while ESC/ERS and PERT further subdivide this group into intermediate-low and intermediate-high risk categories based on the combined imaging and biomarker (cardiac troponin) abnormalities.
- Home-based care and early discharge for low-risk acute PE patients is supported by ESC/ERS, CHEST, NICE, and ASH guidelines. ESC/ERS and ASH suggest using clinical scores (e.g., PESI, simplified PESI, Hestia criteria). CHEST suggests the use of direct oral anticoagulant (DOAC) medications to facilitate home-based care.
- Multidisciplinary PE response teams are recommended by ESC/ERS and PERT. However, these guidelines do not specify which subspecialties are required. ASH acknowledges the growing use of PE response teams along with the lack of high-quality evidence demonstrating improved outcomes.
- ESC/ERS recommend initial anticoagulation with unfractionated heparin (UFH) in patients with suspected high-risk PE. ESC/ERS, PERT, and NICE recommend UFH for hemodynamically unstable PE if advanced therapies (e.g., thrombus extraction, fibrinolysis, or surgery) are being considered. However, recent evidence has demonstrated that fixed-dose low-molecular-weight heparin (LMWH) is associated with a lower incidence of recurrent venous thromboembolism (VTE) and major hemorrhage when compared to UFH.
- In patients with non–gastrointestinal (GI) cancer and PE who do not require UFH, CHEST and NICE recommend the use of a DOAC over LMWH. ESC/ERS and ASH recommend either DOAC or LMWH. CHEST recommends apixaban or LMWH in patients with luminal GI malignancy. ESC/ERS recommends LMWH in pregnant patients with acute PE.
- ESC/ERS suggest that a modest fluid challenge is reasonable in patients with low central venous pressure, guided by invasive monitoring, ultrasound, or clinical monitoring. The guidelines do not discuss the use of a diuretic in normotensive patients with intermediate-risk PE. A universal definition of shock in acute PE is lacking.
- All guidelines recommend fibrinolysis in patients with high-risk PE. All guidelines recommend avoiding routine use of systemic fibrinolysis in intermediate-high risk (submissive) PE due to the risk of major hemorrhage (especially intracranial hemorrhage).
- All guidelines suggest the use of catheter-directed interventions as a rescue treatment following failure of systemic thrombolysis or in individuals with high bleeding risk. NICE suggests that catheter-based embolectomy should be used within the confines of research protocols due to the lack of clinical trial data.
- The most widely agreed-upon indication for inferior vena cava filter placement across all guidelines is for patients with an acute PE and an absolute contraindication to systemic anticoagulation. Other scenarios have marked heterogeneity in guideline recommendations.
- ESC/ERS and PERT recommend a follow-up visit 3-6 months after hospital discharge. ESC/ERS, AHA, and PERT support the use of noninvasive imaging (e.g., echocardiography, 6-minute walk tests, cardiopulmonary exercise testing) to evaluate for the presence of pulmonary hypertension, especially in patients with persistent dyspnea or impaired exercise tolerance >3 months after an acute PE. ESC/ERS, PERT, and AHA recommend referral to a pulmonary hypertension center for further management.
- ESC/ERS, ASH, and CHEST recommend ≥3 months of therapeutic anticoagulation for primary treatment of acute PE. ESC/ERS recommend extended anticoagulation beyond 3 months for patients with persistent or minor transient risk factors. ASH recommends stopping anticoagulation after primary treatment for patients with transient provoking risk factors. ESC/ERS and CHEST suggest DOAC dose reduction for extended-duration treatment (secondary prevention), while ASH suggests either full-dose or reduced dose in this phase.