Review on Cardiac Implantable Electronic Devices: Key Points
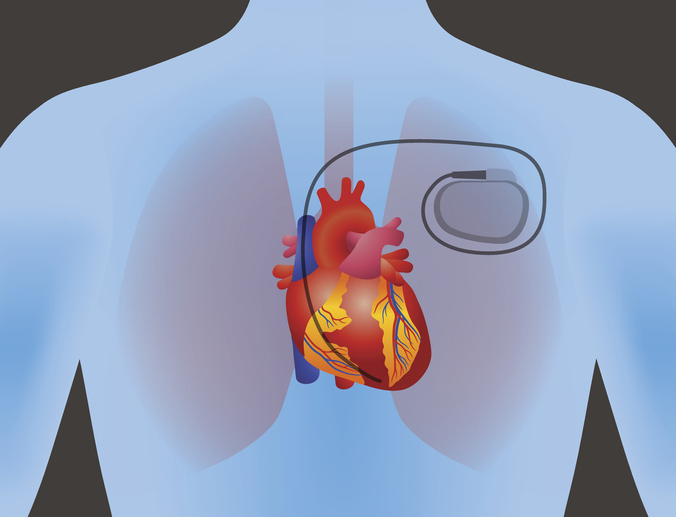
The following are key points to remember from a review article on cardiac implantable electronic devices (CIEDs), which include pacemakers for bradycardia, biventricular pacemakers for heart failure (HF), and implantable cardioverter–defibrillators (ICDs) for the treatment of sudden cardiac death:
Bradycardia pacemakers:
- Bradycardia pacemakers are indicated for sick sinus syndrome and advanced heart block. Single-chamber ventricular pacing and dual-chamber pacing have a similar effect on outcomes in patients with high-grade atrioventricular block. Dual-chamber pacing is preferred for most patients in order to prevent the pacemaker syndrome.
- The leadless pacemaker was developed to avoid pacemaker pocket and lead-related complications. In observational studies, the risk of reintervention or major complications with a leadless pacemaker is lower than the risk with a conventional device, except for the risk of perforation, which is higher in the leadless pacemaker. An important advantage of the leadless pacemakers is the significantly lower risk of infection.
- An important complication of right ventricular (RV) pacing is the development of pacing-induced cardiomyopathy. For patients who are expected to have an RV pacing burden that exceeds 20%, cardiac physiologic pacing, in which the RV lead is positioned in the region of the His bundle or the left bundle branch area, is becoming the standard.
Biventricular pacemakers:
- Class I and class IIa indications for biventricular pacing are grouped as follows:
- An LVEF of ≤35%, left bundle branch block, QRS duration of ≥150 msec, and New York Heart Association (NYHA) class III or ambulatory class IV despite optimal medical therapy for HF;
- An LVEF of ≤35%, left bundle branch block with a QRS duration of ≥130 msec, and NYHA class II, III, or ambulatory class IV despite optimal medical therapy for HF; and
- An LVEF of ≤35%, no left bundle branch block, QRS duration of ≥150 msec, and NYHA class II, III, or ambulatory class IV despite optimal medical therapy for HF.
Conduction system pacing:
- Conduction system pacing involves His bundle pacing or left bundle branch area pacing. Multiple observational and small randomized trials suggest that clinical outcomes are better with conduction system pacing than the traditional cardiac resynchronization therapy (CRT) involving the placement of a coronary sinus lead, although large prospective trials are lacking.
ICDs:
- Indications for an ICD include sustained ventricular arrhythmia or sudden cardiac arrest; chronic systolic HF, an LVEF of ≤35%, and NYHA class II or III despite optimal medical therapy; chronic systolic HF due to ischemic cardiomyopathy, an LVEF of ≤30%; and inherited cardiomyopathies and channelopathies.
- The DANISH trial showed that ICDs used for primary prevention in nonischemic cardiomyopathy did not improve survival. The disparate findings between DANISH and prior trials may be due to selection of patients at higher risk for death from HF than for sudden death from cardiac causes, enrollment of a majority of patients who received a CRT device, and the effects of improved medical therapy for HF. More data are needed on the outcomes of ICD use in patients with nonischemic cardiomyopathy.
- An entirely subcutaneous ICD avoids lead-related issues such as infection, fracture, dislodgement, and tricuspid regurgitation of the traditional devices. The PRAETORIAN and the ATLAS trials showed noninferior efficacy and fewer lead-related complications with a subcutaneous ICD. The main limitation of subcutaneous ICD is its inability to painlessly pace terminate monomorphic ventricular tachycardia.
- To overcome some of the limitations of the subcutaneous ICD (e.g., size and inability to pace), the extravascular ICD was invented, with encouraging initial clinical evidence.
- All currently available ICDs are magnetic resonance imaging (MRI)–conditional (meaning that they are safe in an MRI environment provided that specific conditions are met).
Possible contribution of CIEDs to the clinical presentation:
- Patients who have a CIED and present with any symptom or sign of a systemic infection should be evaluated for a device-related infection.
- Presence of a CIED requires the implementation of the protocolized management plan in the perioperative window, with only a minority of patients requiring assessment by a CIED specialist perioperatively.
- A multidisciplinary approach that involves radiation oncologists, cardio-oncologists, and electrophysiologists is necessary to ensure the safety of patients with CIEDs who are receiving radiation therapy.
Atrial FailureAtrial FunctionalAtrial Functional Mitral Regurgitationcardiaccardiocardio Bloggercardiovascular implantable electronic devicecardiovascular implantable electronic device infectionchest painciedCIED InfectionCIED Infection Prevention and ManagementdiseasesDiuretic Therapy for Patients With Heart FailureECGEmbolic Strokeheartheart diseaseJournal ReviewMavacamten For Obstructive HCMMavacamten For Obstructive HCM: Key PointsMitral RegurgitationMitral StenosisObstructive HCM







